
Sexual Health services
Find sexual health services near you, including sexual health clinics, contraception and abortion services, and sexually transmitted infection (STI) tests and treatment
The Department of Sexual Health and HIV, Nottingham City Hospital runs the HIV outpatient service.
There are clinics running every day of the week. These take place in the GU Medicine building as well as in the Main outpatients building (Clinic 5) at Nottingham City Hospital. A once monthly clinic takes place at the Mary Potter centre in Hyson Green.
These are run by Consultants in Sexual Health/HIV and Infectious Diseases.
To arrange or re-arrange a blood test or hospital appointment please call us on 07812278279.
If you have any queries about your HIV medication (side effects, drug interactions), please contact the HIV specialist pharmacist on 07595284922 or HIV Pharmacist nuhnt.hivpharmacistcallback@nhs.net
They will get back to you as soon as possible during office hours.
If you are expecting a delivery try the delivery company first:
Alcura:
Tel: 08000121551 or 01604433574
E-mail: patientservices@alcura-health.co.uk or Alcura.AlcuraPatientServices@nhs.net
Pharmaxo:
Tel: 01225302188, choose option 1
E-mail: homecare@pharmaxo.com or Pharmaxo.pharmacy@nhs.net
If you have any queries about other aspects of your HIV care, or require some support or guidance relating to HIV, please contact the HIV specialist nurses on CNS email nuhnt.hivcnsreferrals@nhs.net or 07812268514.
They will get back to you as soon as possible during office hours.
SARS-CoV-2 vaccine advice for adults living with HIV: British HIV Association (BHIVA) & Terrence Higgins Trust (THT) guidance - Plain English version
This guidance will develop rapidly; please see the BHIVA website for the latest version
The UK was the first country to approve the use of a COVID-19 vaccine, which is being referred to as ‘The Pfizer vaccine,’ and vaccination with this started on the 8th December 2020. There is also another vaccine, known as ‘the AstraZeneca vaccine’ or ‘the Oxford vaccine,’ which has also been shown to be very effective at preventing COVID-19 and this is currently being assessed for approval. Other vaccines are in the pipeline.
Some of the trials for the two most advanced vaccines have included a small number of people with HIV. There is no reason to think these vaccines will be less safe for people with HIV. Both include some of the genetic material from SARS-CoV-2 (the virus that causes COVID-19) but not the whole virus. This means they are not live vaccines and so are no less safe in people with damaged immune systems.
It is possible that people with HIV might not respond as well to the vaccine. This means that the vaccine might trigger a weaker response in people with HIV. We will monitor any new evidence as it is released and will update this advice if and when needed.
People will receive the vaccine in strict order of priority based on their age, health, occupation, whether they live in a care or residential home and who they live with. Vaccines will be offered strictly based on these priorities. There is no way to jump the queue, and you will be contacted when your vaccine is due.
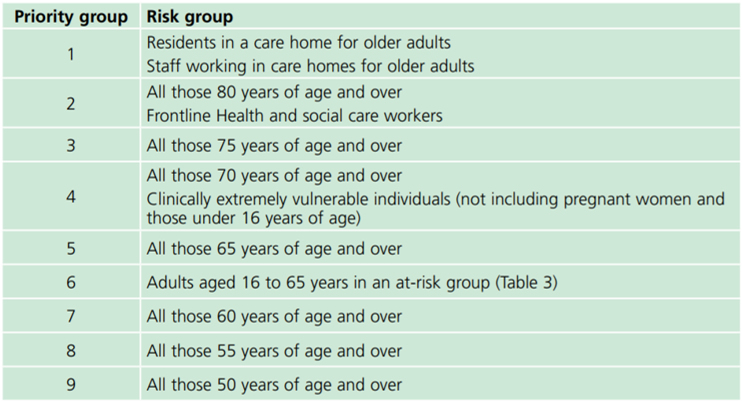
There are 9 priority groups: those in priority group 1 will get the vaccine first, followed by each in turn up until priority 9. After that the vaccine will be offered to everyone else (that is all the people not in priority groups 1-9).
Everyone with HIV is automatically in priority group 6 so you will get the vaccine earlier than many people. If your clinic thinks you are at higher risk you can be put into priority group 4, and get the vaccine sooner, but you will need to be added to a central NHS list to be put into priority group 4. We advise that the people at higher risk may include:
People with a CD4 count less than 50
People with a serious HIV-related illness (e.g. an opportunistic infection) in the last 6 months
People with a CD4 count between 50 and 200 with other issues that increase the risk of getting very sick, such as:
- Detectable viral load
- Low nadir CD4 (the lowest CD4 before starting HIV treatment)
- Other medical conditions associated with increased risk of severe COVID (such as asthma, COPD, diabetes, heart disease, kidney disease, liver disease, Parkinson’s disease, multiple sclerosis, motor neurone disease, conditions or drugs that suppress the immune system (e.g. steroid treatment), severe obesity.
People with ‘multi-morbidity’ meaning that they have other health conditions that may increase the risk of getting very sick.
A full list of the different priority groups:
No, nobody has to have the vaccine. However, we strongly recommend that everyone who is offered the vaccine accepts it. Although vaccine development has been very fast, it has been to the same high standards as any other vaccine trial and includes very careful monitoring of side effects. If anything changes we will update this guidance.
No. It will take many months to vaccinate everyone and it remains important to continue to wash your hands regularly, to wear a mask and to follow your local guidance about social distancing.
Held at NUH's HIV provision
This is a warm, friendly, safe space for open group discussion
Contact our Nurse for the next upcoming meeting!
For further information including location details please contact 07812268514.
NUH are hosting a regular Peer Support Group for people living with HIV. The group is open to all people living with HIV who access NUH for their care.
The sessions are held in a safe, confidential space and are supported by a HIV nurse.
Different topics will be discussed each week and these are chosen by those who attend. If you feel a supportive, understanding and encouraging Peer Support Group is for you then call today.
For further information including location details please contact Nurse Louise Meeson on 07812268514.the number above.